Mucociliary clearance – the respiratory tract’s self-cleaning mechanism
“Mucociliary clearance” (MCC) is of critical importance to general respiratory tract health. As a natural defence mechanism for the lungs, it presents as a key component in the complex network of airway physiology. Amid the challenges posed by obstructive respiratory tract diseases, MCC thus becomes the central focus of therapy. We will explain how mucociliary clearance can be preserved and improved – and lastly, how it helps in the treatment of obstructive airway diseases.

Definition: Mucociliary clearance
Mucociliary clearance describes a self-cleaning mechanism of the bronchi. This term stems from both Latin – ‘mucus’ for phlegm and ‘cilia’ for fluttering hair, as well as from English – ‘clearance’ for purification or removal1. It bases on the coordinated beating of the cilia – very fine, hair-like structures on the surface of the epithelial cells in the respiratory tract. Bronchial phlegm, inhaled particles and the entire coating of the surface epithelium are thus continuously mobilised in the direction of the pharynx, where they are transported outside the body with the aid of tussive clearance such as coughing and the sneezing reflex. Thanks to mucociliary clearance, particles are loosened and removed from the respiratory tract with the aid of secretion formations, demonstrating the essential role that it plays in the clearing of the airways2. It consists of a fundamental physiological cascade of defence mechanisms and gains particular importance in the presence of secretion-forming respiratory diseases.
Mucociliary clearance is not only responsible for continuous clearing of the airways; it also plays a key role in the prevention of acute respiratory tract diseases. Disruptions in this highly-regulated mechanism can result in persistent infections, particularly among patients with previously-existing respiratory tract diseases.
Mist inhalation for bolstering mucociliary clearance
In order to optimise the efficiency of this helpful system, one must first know the conditions under which optimal mucociliary clearance occurs. A temperature of 37°C as well as an absolute humidity of 44 mg/dL, corresponding to a relative humidity of 100%, are required. The effect of even the smallest deviations can be demonstrated on the basis of this example:
Under the above-mentioned optimal conditions, cilia beat with a frequency of approximately 15 beats per second. For mucokinesis, in this case the transport speed of the mucus, this results in segment advancement of 10-15 mm per minute. If the saturation of the water vapour is below 70%, mucociliary clearance will be heavily restricted – here, mucokinesis decreases by a factor of 10. This means that at a starting rate of 10 or more mm/s, particles now move at a rate of only 1 mm/s. If saturation in the trachea is below 50 percent, this can even result in a disruption of the process, as shown in this video:
You are currently viewing a placeholder content from YouTube. To access the actual content, click the button below. Please note that doing so will share data with third-party providers. More Information
- Drying out of the mucosa
- Loss of cilia activity which may slow down mucokinesis
- Thickening and retention of secretions
- Ulceration of the mucous membranes
The RC-Cornet® PLUS is an oscillating PEP therapy device for the lower respiratory tract that features an integrated mist inhalation connection, thus combining both of these approaches. It offers effective support for expectoration, reducing coughing and shortness of breath in the process.
Respiratory therapy + mist inhalation
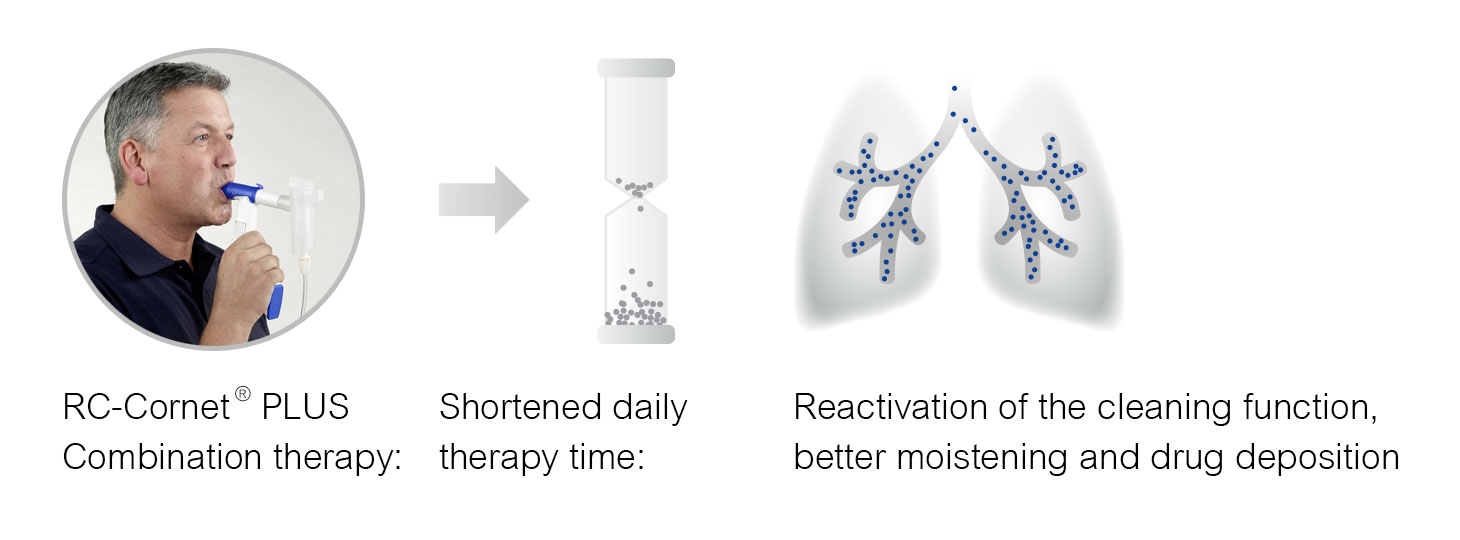
RC-Cornet® PLUS
PEP therapy device with oscillation and connection for mist inhalation
1 Verband Pneumologischer Kliniken e.V. (VPK), o.D. Glossar – Mukoziliäre Clearance. Lungenärzte im Netz. Abgerufen bei https://www.lungenaerzte-im-netz.de/nc/glossar/source/default/term/mukoziliaere-clearance/ am 14.11.2023
2 Oczenski, W. (2017). Atmen–Atemhilfen. 10. überarbeitete und erweiterte Auflage, S. 339ff.
3 Weise, S., Kardos, P., Pfeiffer-Kascha, D., & Worth, H. (2019). Empfehlungen zur Atemphysiotherapie (p. 14). München, Orlando: Dustri-Verlag Dr. Karl Feistle.
4 Oczenski, W. (2017). Atmen–Atemhilfen. 10. überarbeitete und erweiterte Auflage, S. 339ff.
5 Merz, P. (Ed.). (2021). Physiotherapie in der Inneren Medizin. Nicht invasive Beatmung. Georg Thieme Verlag. S. 344ff.
6 Cegla, U. H., Jost, H. J., Harten, A., Weber, T., & Wissmann, S. (2002). Krankheitsverlauf bei schwerer COPD mit und ohne physiotherapie mit dem RC-Cornet®. Pneumologie, 56(07), 418-424.
Foto: GlobalStock / istock.com
Regularly well informed:
- Free of charge and sent easily via e-mail
- You can unsubscribe at any time

