Long-COVID and post-COVID

© Shutterstock/ SB Arts Media
What exactly are long-COVID and post-COVID?
While most affected persons experience a complete recovery only a few weeks after an infection, some others suffer from symptoms for a much longer time – or they experience the development of symptoms only after a certain period of time. Based on our current state of research, it is still difficult to ascertain the reason. In a study in Great Britain involving about 20,000 patients, symptoms were identified in 13.7 % of patients 12 weeks after the infection.1
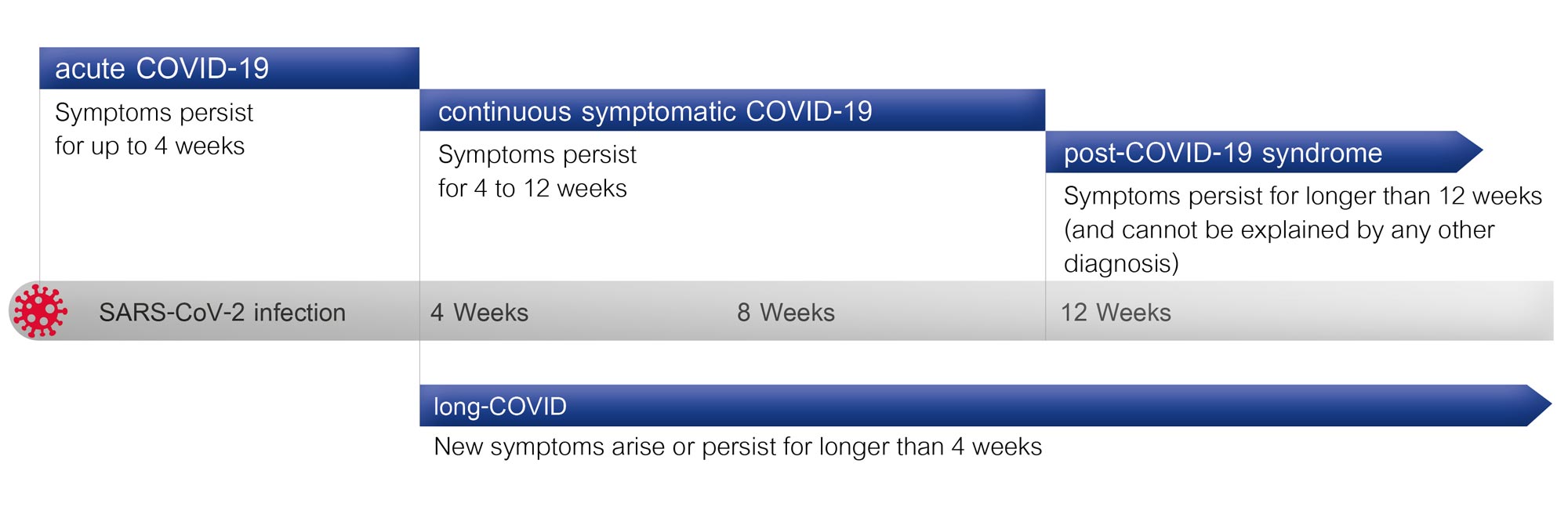
Fundamentally: According to current guidelines, if symptoms are still present up to 28 days after infection, this is considered an acute infection. A continuous, symptomatic COVID-19 infection is thus present when the symptoms last for up to 12 weeks, but remain the same. We speak of post-COVID only when symptoms that cannot be explained by any other cause, are still present after 12 or more weeks. The term long-COVID is used, in contrast, when the symptoms are present for longer than four weeks after the infection, or even when new symptoms arise.2
What symptoms arise with long-COVID and post-COVID?
In general, long- and post-COVID manifest as a multitude of symptoms that have a severe effect not only on the lungs, but also on the general health of affected persons.
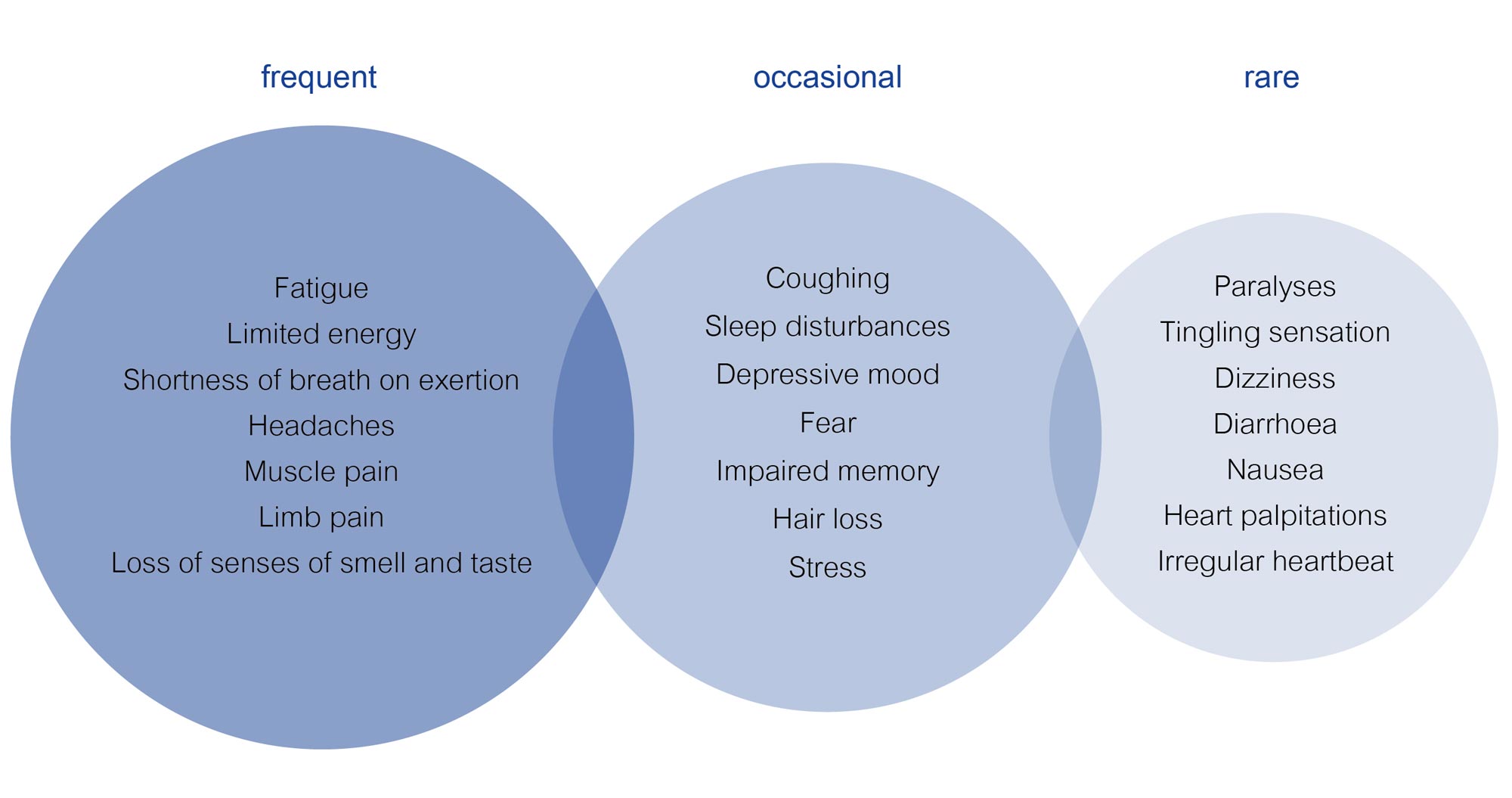
Symptoms associated with long- and post-COVID are numerous.
- The most prominent is exhaustion – also known as chronic fatigue. It commonly occurs following a debilitating disease or treatment, such as with a cancer diagnosis. The exact causes are unknown, which also makes therapy more difficult. Classic physical and psychological symptoms are premature fatigue, even when performing small everyday tasks such as light housework or shopping. As a result, affected persons feel a lack of motivation and interest, and find that rest brings them restoration only rarely or very slowly. In some cases, lack of concentration, speech difficulties and forgetfulness may also be experienced.3
- The other most common symptoms mentioned above, include symptoms such as breathing difficulties, shortness of breath, and a loss of smell and/or taste. Even after official recovery, the infection may be accompanied by ongoing damage to the lungs, shortness of breath, and a reduced oxygen supply. Accordingly, many patients must battle shortness of breath (dyspnoea) on exertion.
- In contrast, symptoms such as dizziness, nausea, diarrhoea, loss of appetite, ear pain, etc., have been observed rather infrequently.
- Beyond fatigue, there are additional psychological symptoms that can be triggered or intensified due to long- or post-COVID: Affected persons often exhibit signs of increased anxiety or even depression.
- Muscle weakness and pain are also experienced in some cases.
Some long-term effects arise frequently after the acute phase of the illness:
- A worsening in lung function
- Further complications in other organs such as inflammation of the heart muscle
- Renal and metabolic diseases such as diabetes mellitus, commonly known as diabetes
- Thromboemboli – the clogging of a vessel by a blood clot 4

Fatigue is a word of French origin that is used with similar meaning in both English and German. It stands for extreme tiredness or exhaustion that is experienced both physically and mentally.
How are long-COVID and post-COVID treated?
The list of possible symptoms that accompany long- and post-COVID is long. Even in terms of the affected organs, this medical condition is characterised by its diversity: From the lungs, to the heart, and on to the brain – long- and post-COVID can affect multiple parts of the body simultaneously. Treatment must be designed to be accordingly flexible – and it must be adapted to the possibly changing symptoms.
In terms of the primary symptom of fatigue, which affects both the body and the psyche to a large extent, a combination of light strength and endurance exercises is currently considered as a therapeutic approach. Overexertion should be avoided in every case. Thus, therapy should always be conducted in consultation with a doctor. The scope and intensity should only be increased very slowly. Patience and time are requirements for this therapy. According to studies, the basic symptoms improve gradually after 3-6 months, especially as pertains to shortness of breath.
How can the lungs be treated during COVID and later with long- and post-COVID?
As early as during the acute phase of the coronavirus, affected persons often feel abruptly tired and defeated. A high fever and dry cough also appear quickly. Viruses are the reason. Due to their fast propagation, the respiratory organs are first impacted as viruses normally arrive in our bodies through the respiration. Especially with Omicron variants, infections of the upper respiratory tract (nasopharyngeal infections) also occur frequently. The obstruction of the airways with mucous and the thus-resulting tension headache are often depicted under this variant as being unbearable. Even medication intended for migraines is unable to provide help. In this case, a treatment option is oscillating respiratory therapy devices, especially for the upper respiratory tract, such as the RC-Cornet PLUS® NASAL. These are able to release stubborn phlegm. The tension headache is eased. In addition, these are able to moisten the airways via inhalation and thus support recovery.
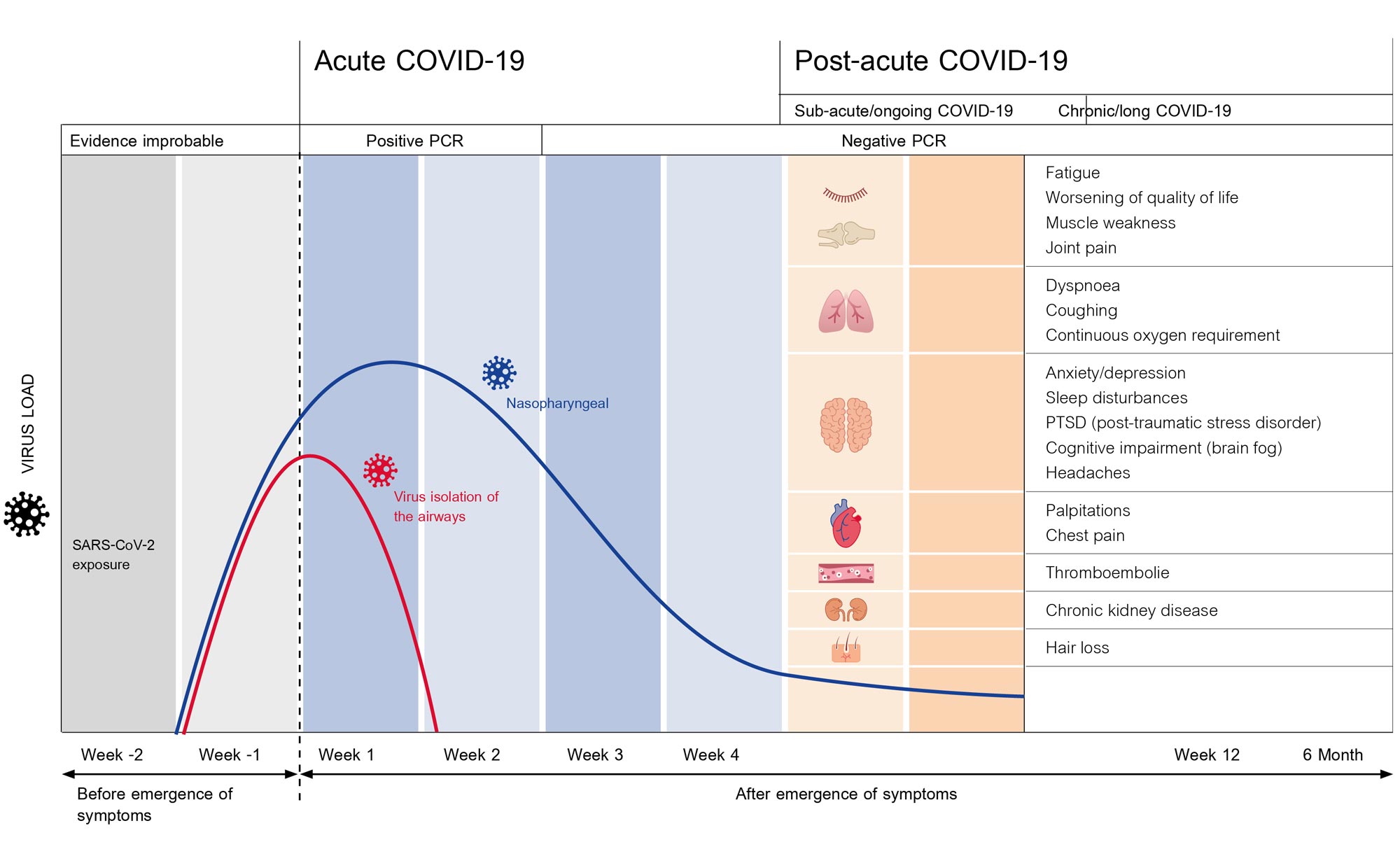
Progression of a COVID-19 infection (Source nocovid_pcs.pdf (nocovid-europe.eu)
It is not only the upper airways that are severely attacked by the virus during this time. The lower airways, our lungs themselves, are in part heavily compromised by the disease. Known effects: lung function worsens. This manifests in patients through shortness of breath or even dyspnoea on exertion or via pulse oximeter, often also through a reduced oxygen saturation, even while at rest. Many patients, especially those of advanced age, must go to hospital.
According to current S1 guidelines, the first step for patients requiring intensive care consists of ventilation or oxygen supplementation if appropriate.5 Such a guideline is developed by an expert committee in collaboration with other professional societies and organisations, in order to derive common treatment recommendations. A delimitation to an S2 or S3 guideline occurs when consensus is found in a rather informal procedure, possibly because a new illness has arisen and a systematically-developed approach to therapy does not yet exist.
Here, patients are given support for strengthening of the respiratory muscles and for a clearing of the airways through a targeted combination of exercises and therapy, while still in hospital. With COVID-19, a disruption in diaphragmatic breathing (abdominal breathing) also occurs often, and must be trained accordingly.

Among other things, the approaches of Respiratory Muscle Training (RMT) , which have been tried and proven for decades, have shown to be helpful in supporting the rebuilding of the respiratory muscles. This concept includes methods such as “pursed lips”, diaphragmatic breathing, or light conditioning training – accompanied, as needed, by supportive techniques that can facilitate the expectoration of mucus. A study with about 80 coronavirus patients, who underwent a six-week programme with elements of respiratory training and therapy, showed a clear result: A tripling of the FVC value, an indicator for the measurement of lung volume. While 35 % of participants reported having trouble with expectoration at the start of the study, it was possible to reduce this value to 5 %. While 50 % of study participants initially complained of shortness of breath, this number decreased to only 15 % at the end of the study.6
What is the best way to avoid long-COVID and post-COVID?
A study of approximately one million double-vaccinated participants in the United Kingdom demonstrated that the probability of suffering under the typical symptoms of a coronavirus infection for longer than 28 days, decreased with the vaccination by 49 %.7
Patients with long-COVID and post-COVID also benefit from inspiratory muscle training (IMT) when using respiratory training and therapy devices: Resistance breathing strengthens the inhalation and exhalation muscles, which are often dramatically weakened by a COVID-19 infection, and which require strengthening and training. Thus, a study with 42 participants demonstrated clearly improved lung function values and a decrease in respiratory problems, while the control group without IMT showed none of these effects.8
The RC-FIT® was especially developed for such uses. It is designed for training and therapy of the airways and makes use of IMT methods, among others. Here, a variable resistance is created with the help of a vibration plate, which trains the respiratory muscles. Especially with the primary symptom of fatigue, a gentle endurance training has proven useful in returning patients to their normal performance levels. Here, the RC-FIT® can provide optimal support.
Respiratory therapy and respiratory training with oscillations and sounds
The RC-FIT® combines the proven approaches of IMT and oscillation. The gentle vibrations help with expectoration of the mucus and clearing of the airways. Thanks to the resistance, the respiratory muscles are exercised and the respiratory rate is reduced, producing a calming effect on the breath and the psyche.
The RC-FIT® provides valuable support in the rehabilitation and training of the airways. It combines therapy concepts that have been long tested and documented through studies and guidelines, and it gradually helps patients to breathe deeply once again.
Studies clearly demonstrate the important role that IMT, OPEP, and related therapies play in the treatment of long-COVID and post-COVID:
- Oscillations loosen the secretions in the airways
- The airways are kept open, thus improving the ventilation of the lungs
- The respiratory muscles are exercised
- Shortness of breath can be reduced, which has a calming effect on the nervous system
Especially for long- and post-COVID patients, these effects are crucial when it comes to treatment of the (ongoing) symptoms. The RC-FIT® CLASSIC product combines the advantages of IMT and oscillations – it helps to free the airways from mucus and it helps to exercise the respiratory muscles through a variable resistance. It is thus an optimal form of support for the rehabilitation of the lungs – whether at home or under the instruction of medical personnel. The RC-FIT® CLASSIC is easy to use and is applicable for a multitude of indications and situations.
1 Ayoubkhani, D., Pawelek, P. & Gaughan, C. (2021). Technical article: Updated estimates of the prevalence of post-acute symptoms among people with coronavirus (COVID-19) in the UK: 26 April 2020 to 1 August 2021. Office for National Statistics.
2 Deutsche Atemwegsliga e.V., 2021: S1-Leitlinie Post-COVID/Long-COVID. Abgerufen über https://www.atemwegsliga.de/aktuell/s1-leitlinie-post-vovid-long-COVID.html am 03.02.2022
3 MEDICLIN Kraichgau-Klinik, 2022: Krankheitsbild: Fatigue Syndrom. Retrieved via https://www.kraichgau-klinik.de/fachbereiche-krankheitsbilder/onkologie/fatigue-syndrom/#was-ist-das-fatigue-syndrom am 06.05.2022
4 Infektionsschutz.de, 2022: Long COVID: Langzeitfolgen von COVID-19. Retrieved via https://www.infektionsschutz.de/coronavirus/basisinformationen/long-covid-langzeitfolgen-von-covid-19/ am 09.05.2022
5 Koczulla, A. R., Ankermann, T., Behrends, U., Berlit, P., Böing, S., Brinkmann, F., … & Zwick, R. H. (2021). S1-Leitlinie Post-COVID/Long-COVID. Pneumologie, 75(11), 869–900.
6 Kołodziej, M., Wyszyńska, J. & Bal-Bocheńska, M. (2021). COVID-19: A New Challenge for Pulmonary Rehabilitation? Journal of clinical medicine, 10(15), 3361. https://doi.org/10.3390/jcm10153361
7 Antonelli, M., Penfold, R. S., Merino, J., Sudre, C. H., Molteni, E., Berry, S., … & Steves, C. J. (2022). Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case-control study. The Lancet Infectious Diseases, 22(1), 43–55.
8 Abodonya, A. M., Abdelbasset, W. K., Awad, E. A., Elalfy, I. E., Salem, H. A. & Elsayed, S. H. (2021). Inspiratory muscle training for recovered COVID-19 patients after weaning from mechanical ventilation: A pilot control clinical study. Medicine, 100(13).
9 Suggett, J. & Kushnarev, V. (2021). Oscillating Positive Expiratory Pressure (OPEP) Devices and Airway Clearance Therapy in the COVID-19 Patient Care Pathway: A Review of Where There May Be Clinical Value. TP117. TP117 COVID-19 PATHOPHYSIOLOGY AND MODELLING, A4477-A4477.
Weitere:
• Physio Assist, 2021: Post-/Long-COVID Leitline – Schwerpunkt Lunge Webinar 27.10.21 – PhysioAssist. YouTube. Retrieved via https://www.youtube.com/watch?v=Y0JjVEr3FEw am 02.02.2022
• Better Breathing, 2022: REHABILITATION After COVID-19. Retrieved via https://betterbreathing.ie/rehabilitation-after-COVID-19/ am 28.01.2022
Subscribe to our
BREATHE EASY Newsletter
Tips and information on healthy airways!
- for all who wish to breathe better
- free of charge and convenient e-mails
- compact newsletter once a month
For all those who deal with pneumological topics related to the respiratory tract in a professional context, please find here the subscription to the CEGLA FACHNEWSLETTER.