Expectoration and secretion mobilisation with oscillating therapy

Definition: Expectoration via oscillation
Oscillatory therapy uses mechanical vibrations to loosen secretions in the airways and facilitate their removal. This therapy triggers a resonance phenomenon that, among other things, oscillates the bronchial tree. The effect is that the viscous secretions are loosened from the bronchial walls, transported from a distal to central direction, and are thus more easily suctioned or coughed out1.
The oscillating PEP (positive expiratory pressure) makes use of both the oscillations and the proven method of expiratory resistance. These cause the respiratory tract system to open, which supports mucociliary clearance2. Multiple studies have confirmed the effectiveness of oscillating PEP therapy for pulmonary diseases, such as COPD. Thus, in addition to assisting with expectoration, this therapy can help to increase reduced pulmonary volumes, reduce hyperinflation of the lungs, and ensure an improved exchange of gases3. OPEP has become a frequently-used procedure in pulmonary therapy.
Expectoration in inpatient treatment settings
Expectoration is used in clinical settings, among other things, for patients who have problems with expulsion of secretions, possibly due to weakness or because the mobilisation of secretions is made more difficult due to their lying-down position. To this end, there are different procedures and techniques from the field of modern respiratory physiotherapy that can provide remedial action. Studies have shown that expectoration through oscillatory PEP (OPEP) can result in clearly improved auscultation findings after only 14 days, following five minutes of use three times a day. In addition, OPEP has produced significant improvement of vital capacity and FEV1 (forced expiratory volume in 1 second), as well as of peak flow value4.
Another study on 50 inpatients with serious COPD demonstrated that the consistent use of OPEP could shorten the length of hospital stays. With a pure drug-based treatment, patients remained in hospital an average of 18.3 days. With a combination of OPEP and drug-based treatment, this was only 16.2 days. Further, in the trial group only 13 patients required antibiotic treatment while in the control group it was 24 out of 25 patients5.
Oscillations can even be useful for expectoration among tracheostomised patients with cannulae. One such example is the RC-Cornet® PLUS TRACHEO. It provides an additional option for simultaneous inhalation therapy and can be used independent of position, making the suction of secretions easier.
Overall, OPEP demonstrably contributes to a reduction in dyspnoea, thus helping patients to breathe better. The easy use of this auxiliary device also supports nurses when assisting patients with the expulsion of secretions6.
Contribution by NDR Magazine, showing its use in daily clinical care:
Expectoration in outpatient therapy
The expulsion of secretions also plays an important role in outpatient care. Special devices that allow for easier suctioning or expectoration are made available to patients and their caregivers, and can thus alleviate the symptoms of illness. These include, for example, the RC-Cornet® PLUS, an oscillating PEP therapy device for the lower respiratory tract. It helps affected persons to loosen up mucus, it reduces coughing, and alleviates shortness of breath. In turn, this reduces the risk of exacerbations and the need for antibiotics7.
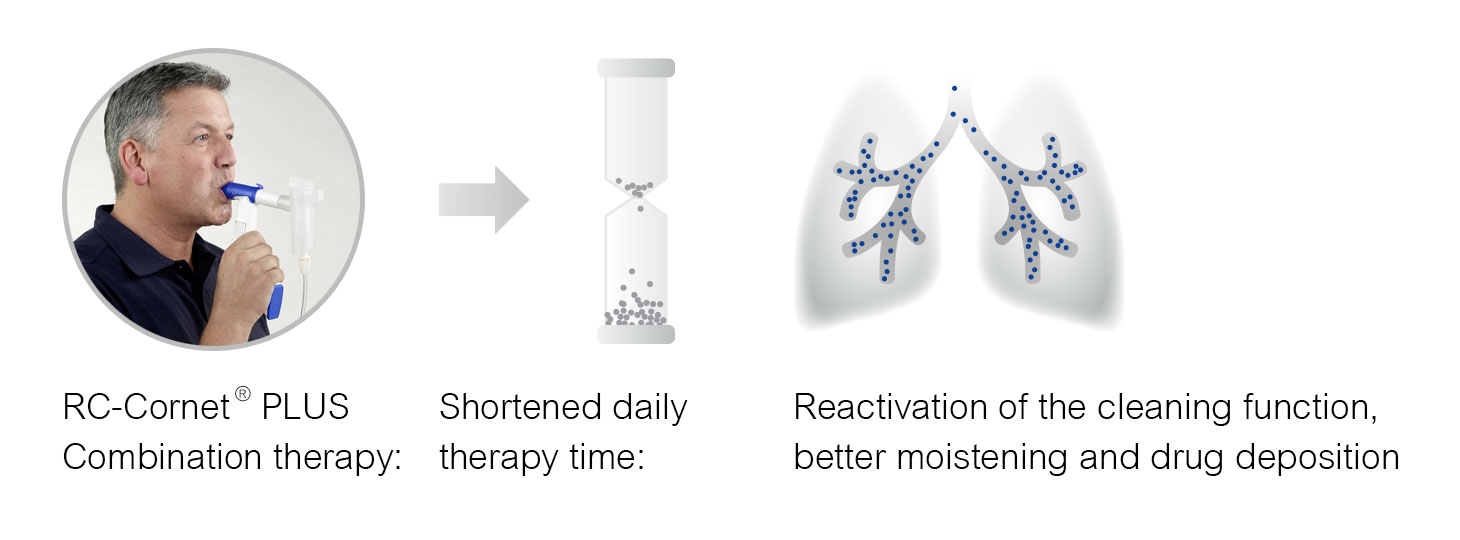
The RC-Cornet® PLUS can also be used in combination with mist inhalation, by connecting the integrated nebuliser attachment to the inhalation device. This option can improve drug deposition and shorten the therapy time – an important criterion for outpatient therapy. A randomised study of 35 patients with serious COPD showed that, following inhalation of identical drug dosages, significantly better pulmonary function was found in the group that used an oscillating PEP system as part of inhalation therapy. As a result, their therapy time was also shortened8.
The oscillating PEP method can provide remedial action in an outpatient setting and thus impart affected persons with a generally better attitude to life.
Oscillating PEP for expectoration at home
Most importantly, expectoration is an important component of therapy for chronic pulmonary diseases. In this field, medical specialists have a number of techniques available to them such as inhalations, respiratory physiotherapy, and oscillating PEP devices. These methods can provide relief of symptoms, especially among patients with sticky and especially stubborn mucus. OPEP helps by liquefying secretions and facilitating breathing.
An advantage from the point of view of private-practice pulmonologists is that, when using OPEP therapy for expectoration issues, hospital referrals are much more rare. This was demonstrated in a study of 50 patients with serious COPD who were observed for more than two years9.
RC-Cornet® PLUS has also proven its worth during home use, as it can be easily used by both adults and children following first-time instruction on its use by practice personnel. Thus, it has been scientifically proven to assist with gentle secretion mobilisation and with successful secretion management.
Summary
Oscillatory therapy offers a promising treatment option for patients with (obstructive) respiratory tract diseases, especially those with viscous secretions. There is great potential in this area, especially with the use of oscillations and oscillating PEP. Thanks to mechanical oscillations, secretions can be effectively loosened and their removal made easier. This leads to an improvement in respiratory function and quality of life. Furthermore, oscillatory therapy generally does not produce any side effects and can be used by both adults and children.
1 App E M, Wunderlich M O, Lohse P, King M, Matthys H. Oszillierende Physiotherapie bei Bronchialerkrankungen – rheologischer und antientzündlicher Effekt. Pneumologie. 1999; 53 1-12
2 Ramos, F. L., Krahnke, J. S., & Kim, V. (2014). Clinical issues of mucus accumulation in COPD. International journal of chronic obstructive pulmonary disease, 139-150.
3 Kähler, K. (2020). Der Einsatz von oszillierenden PEP-Systemen (hier RC-Cornet® PLUS TRACHEO) bei tracheotomierten Patienten im Rahmen des Weanings. Bildungszentrum für Gesundheitsberufe Asklepios Hamburg, Fort- und Weiterbildung Anästhesie und Intensivpflege.
4 Fagevik Olsén M, Lannefors L, Westerdahl E. Positive expiratory pressure – Common clinical applications and physiological effects. Respir Med. 2015 Mar;109(3):297-307. doi: 10.1016/j.rmed.2014.11.003. Epub 2014 Nov 12. PMID: 25573419.
5 Merz, P. (Ed.). (2021). Hilfsmittel und apparative Unterstützung. Physiotherapie in der Inneren Medizin. Georg Thieme Verlag, 175-208.
6 Nationale Versorgungsleitlinien (2021). 4 Nicht-medikamentöse COPD. NVL COPD. Abgerufen bei https://www.leitlinien.de/themen/copd/2-auflage/kapitel-4 am 24. Juli 2023.
7 Cegla U H, Retzow A. Physiotherapie mit dem VRP1 bei chronisch obstruktiven Atemwegserkrankungen – Ergebnisse einer Multizenterstudie. Pneumonie. 47; 1993 636-639
8 Cegla, U. H., Jost, J. H., Harten, A., & Weber, T. (2001). RC-Cornet® verbessert den Effekt einer Inhalationstherapie mit Ipratropiumbromid (Atrovent®) bei COPD-Patienten. Pneumologie, 55(10), 465-469.
9 Cegla, U. H., Jost, H. J., Harten, A., Weber, T., & Wissmann, S. (2002). Krankheitsverlauf bei schwerer COPD mit und ohne Physiotherapie mit dem RC-Cornet®. Pneumologie, 56(07), 418-424.
Other:
• Cegla, U. (2000). Physiotherapie mit oszillierenden PEP-Systemen (RC-Cornet®, VRP1®) bei COPD1. Pneumologie (Stuttgart, Germany). 54. 440-6. 10.1055/s-2000-7685.

